I'm Having Orthopedic Surgery
Reducing Pain and Improving Outcomes
- PAA anesthesiologists are experts in the selection, placement, and management of nerve blocks.
- The nerve block placed by your PAA anesthesiologist will allow you to have a more comfortable surgical experience, recover more quickly, and reduce your need for opioid medications.
- PAA has a team of anesthesiologists who provide specialist care in the area of orthopedic and regional anesthesia.
- One of our physicians with extensive regional anesthesia experience is available 24/7 to answer questions and concerns you may have about your nerve block.
What The Experts Are Saying
Frequently Asked Questions
What is regional anesthesia?
Regional anesthesia is a type of anesthesia where one part of your body is made numb by local anesthetics, also known as numbing medication. There are two categories of regional anesthesia – peripheral nerve blocks and neuraxial anesthesia (spinals and epidurals). Depending on the type of surgery you’re having, you may be able to have one or both types.
Peripheral Nerve Blocks – Your anesthesiologist will use an ultrasound to find clusters of nerves and inject numbing medication around them. This stops sensations from that particular area of your body, blocking pain signals from reaching your brain. We’re able to target nerves in the arm, legs, abdomen and chest. You may have a one time dose of numbing medication or a catheter (a tiny plastic tube) placed, depending on your surgery and medical history.
Who will perform the nerve block and/or neuraxial anesthesia?
What can I expect on the day of surgery if I'm getting a peripheral nerve block?
How long does a nerve block last?
How long a nerve block lasts depends on the type of numbing medication used as well as if you had a single shot block or a catheter placed. A single shot nerve block is when only one dose of medication is left near the nerves. Typically, you can expect 6-18 hours of numbness with this type of injection, however some patients may remain numb for up to 24 hours or more. If a single shot block was performed with EXPAREL you may have longer lasting effects (see the FAQ specifically related to EXPAREL below).
If a catheter is placed, it means that a small plastic tube was left near the nerves and numbing medication can be infused over the course of 2-4 days. For safety reasons, the numbing medication that is infused is a lower concentration than the initial injection. This means, when you have a nerve catheter, 12-24 hours after the initial placement of the nerve block, you’ll likely begin to notice increased sensation in the part of your body affected by the nerve block. You may experience a sensation of “pins and needles,”mild to moderate aches, or even begin to regain the ability to move the affected extremity.
This does not mean that the nerve catheter is no longer working. Your nerve catheter is still decreasing your pain level a great deal, and you’ll be prescribed oral pain medications by your surgeon to help manage any increased discomfort. It’s safe to take oral pain medications while a nerve catheter is in place.
Does having a nerve block mean that I'll be awake during surgery?
Is it safe to get a nerve block?
Risks associated with nerve blocks include, nerve injury, bleeding, infection, soreness, allergic or other reactions, changes in blood pressure, heart rate, and damage to structures surround the nerves (such as the lung and major blood vessels). In order to reduce these risks, we perform our nerve blocks under ultrasound guidance. We also place the nerve blocks before you’re completely asleep, so that you may alert us if you have any painful or uncomfortable sensations. Your vital signs will be monitored during and after the procedure to ensure your safety, too.
What are some of the side effects?
After a nerve block, it’s expected to have numbness or tingling in the area of the block. You may also have muscle weakness. If you had a block for the arm or shoulder you may experience a change to your pupil size (on the side of the block) or drooping of your eyelid (ptosis). This is called Horner’s Syndrome. In addition, a stuffy nose or hoarseness in your throat may occur.
You may experience mild shortness of breath or feel like you cannot take a deep breath. This is due to the fact that the nerve that goes to the diaphragm is surrounded with numbing medication along with the nerves that go to the arm. This type of sensation is normal and it’ll resolve as your block resolves, too.
What is a nerve catheter? How do I care for my nerve catheter?


Your catheter will be taped in place with clear on white tape. The location of your catheter will depend on the type of block you received. The ball that holds your numbing medication will be kept in a bag with a strap so you can move around easily while you recover.

What are some common issues with nerve catheters? When and how do I remove my nerve catheter?
What are some common issues with nerve catheters?
Leaking: You may have some leakage of fluid around the catheter. This may be clear or may appear to have some blood in it. As long as your pain is under good control, this is nothing to worry about. You may reinforce the dressing over your catheter with tape if needed.
Disconnection: If the small plastic tubing becomes disconnected at the yellow clamp, please call us to discuss your options. We may be able to walk you through reconnecting it, have you come to the hospital for us to help you, or we may suggest you remove the catheter depending on the situation.

This yellow clamp is the most common area for disconnection.
Side Effects: There are some expected and common side effects (see FAQ “What are some of the side effects” above). If you’re experiencing any of these please let us know. In most cases, we can provide reassurance that these are normal side effects, however, if you have concerns about symptoms that are intolerable or worsening, please reach out to us. Additionally, if you’re experiencing unbearable side effects, you can clamp the catheter with the small white clamp (located on the tubing) to stop the flow of medication. In an emergency, call 911 or proceed to an emergency room.
Pain: When you are initially given a nerve block, a strong numbing medication is used that typically makes you very numb. The medication in the pump/ball is less strong for safety reasons. This means that once the initial block wears off you may start to notice less weakness, an increase in sensation, and even slight amounts of pain. This is expected. While your pain may increase somewhat, it should still be tolerable and the nerve catheter will continue to significantly reduce the amount of pain you experience. You’ll be able to take oral pain medications along with the nerve catheter. If you feel your pain is uncontrollable, check the tubing to make sure all clamps are open, that there are no kinks and that no part of the catheter or pump are disconnected. We can help you troubleshoot over the phone and discuss your options if you run into any issues.
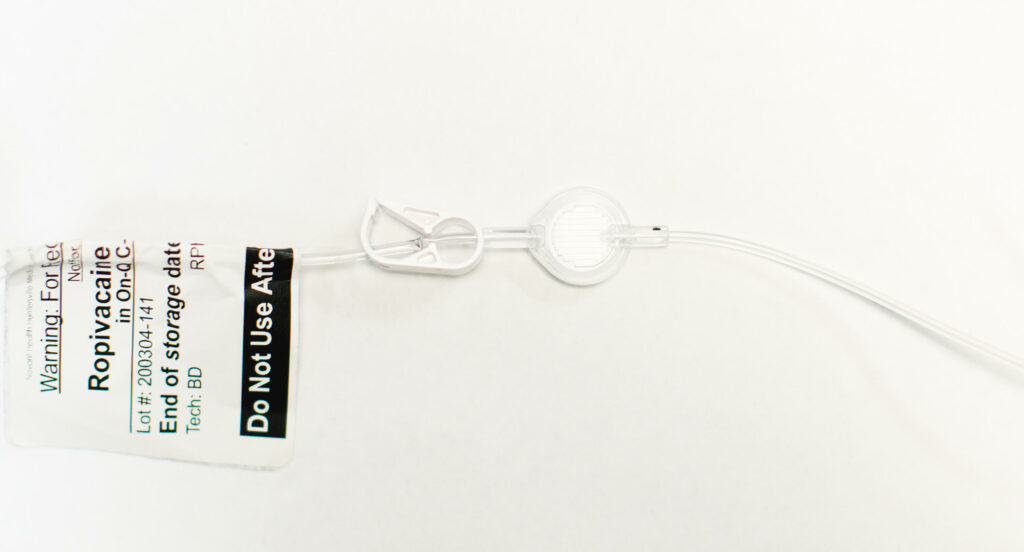
Ensure this white clamp is open so that your numbing medication can flow freely.
When and how do I remove my nerve catheter?
When the infusion of medication is complete, the ball will look like an apple core or a flat pancake. At this point, you may remove the catheter. Be sure to wash your hands prior to removal. To remove it, carefully peel back the dressing and loosen the strips of tape over the catheter. Hold the tubing close to the skin and gently pull until the catheter is out of the body. The catheter should slide out easily and it will have a blue tip at the end. If you do not see a blue tip or if it seems difficult to remove, please call us right away. After removal, place a small bandage over the site where the catheter was in place. The tubing and ball can be thrown away.

Your ball will look like this when it is full of numbing medicine.

Your ball will look like this when the infusion is complete. You’ll remove it at this point.

After you remove your catheter, you should see that the end has a blue tip.
Who do I contact if I have issues with my nerve catheter?
What if my doctor chooses to use EXPAREL for my nerve block?
- EXPAREL is a single dose medication, so you will not go home with a nerve catheter in place
- EXPAREL contains specially formulated bupivacaine (a type of local anesthetic) that is designed to release into your body over a long period of time for lasting pain relief.
- The motor effects of EXPAREL typically wear off after 12-24 hours and you may feel some increased pain at this time. This does not mean the block isn’t working. Instead, it is transitioning from a higher concentration to a longer acting, lower concentration.
- After the first 24 hours, the sensory effects of the nerve block range from very subtle to distinct numbness or tingling in a particular body part. Depending on the location of the nerve block, 3+ days is not uncommon, and you should not be alarmed. 7 days has even been seen in rare instances.
- Because EXPAREL works overtime, you may need fewer doses of other medications including opioids.
- For more information about EXPAREL click here
